There are several benefits for organizations that are granted nonprofit, tax exempt status by the US Internal Revenue Service (IRS); however, with those benefits come additional responsibilities. That’s because an organization’s nonprofit status rests in the general law of charity. A tax-exempt organization must be organized and operated exclusively for exempt purposes—one of which is charitable. In the context of operating a tax-exempt hospital, it’s not enough for a hospital to state that it operates exclusively to promote health. A hospital must also demonstrate that it operates to promote the health of a class of persons that is broad enough to benefit the community. This is known as the community benefit standard.
For example, a nonprofit healthcare organization licensed by the state as a hospital must serve the best interest of the entire community it serves, not just the patients that receive care and services from the hospital. For instance, if the hospital operates an Emergency Department (ED), the ED must accept all patients regardless of their ability to pay and not just patients referred to the ED by a medical group owned by the hospital. The former improves access to care for the whole community while the latter improves access to care only for those in whom the hospital has a private interest.
Hospitals with 501(c)3 tax-exempt status must demonstrate to the IRS that they meet the community benefit standard. Each year, nonprofit, tax-exempt hospitals must report to the IRS on the activities and policies of, and community benefit provided by, its hospital facilities and other non-hospital health care facilities that it operated during the tax year provided to the community on the Form 990, Schedule H. To identify the community needs that can be served hospitals must begin by conducting a Community Health Needs Assessment (CHNA). The CHNA is a federal requirement that must be conducted every three years. Once the community needs are known and understood, hospitals must determine what needs it is able to address and how it will do so. This is documented in the Community Health Improvement Plan (CHIP). Then these activities and initiatives must be tracked and reported.
Often ensuring compliance with these requirements is viewed as an administrative function; therefore, some hospital leadership and staff do not understand these requirements and what their role is in helping the hospital achieve compliance. And compliance is critical. Failure to meet these standards may result in revocation of the organization’s tax-exempt status and excise taxes imposed as fines. While few hospitals have their tax-exempt status revoked, many hospitals are audited as a result of issues with submissions which often results in additional costs to the hospital.
There is a renewed interest at the federal level in ensuring that tax-exempt hospitals are meeting the intent of the community benefits standard. Senator Chuck Grassley, chair of the Senate Finance Committee, was the impetus for changes to the tax code that instituted initial reporting requirements for tax-exempt hospitals back in 2008. Grassley has retaken his seat as the chair of the Committee and revived his oversight of this issue last month with a letter to IRS Commissioner Charles Rettig, asking for a briefing on the full scope of the agency’s audits. It is therefore critically important that tax-exempt hospitals and their staff understand and engage in the process to achieve compliance.
In this article, we provide information to educate hospital staff and leaders about these requirements by:
- Defining community benefits
- Explaining the purpose and process for the CHNA and CHIP, and
- Advising hospital leadership on approaches to ensure that staff are regularly and accurately reporting qualifying activities
Community Benefits
A Community Benefit must respond to an identified community need and meet at least one of the following criteria:
- Improve access to health care services
- Enhance health of the community
- Advance medical or health knowledge
- Relieve or reduce the burden of government or other community efforts
A program or activity should not be reported as community benefit if it is:
- Provided for marketing purposes
- Restricted to hospital employees and physicians
- Required of all health care providers by rules or standards
- Questionable as to whether it should be reported
- Unrelated to health or the mission of the organization
Categories of community benefits and associated activities may include: Research (e.g., clinical, community health); Health Professions Education (e.g., physicians; medical students; nurses; nursing students, scholarships; funding for education); Community Health Services (e.g., health education, clinical services); Subsidized Health Services (e.g., emergency and trauma services, hospital outpatient services, behavioral health services, palliative care and hospice) Community Building (e.g., physical improvements and housing, economic development, environmental improvements, coalition building); Financial and In-kind Contributions (e.g., cash donations, grants, in-kind donations); Community Benefit Operations (e.g., dedicated staff, community health needs and assessments).
According to the Catholic Hospital Association (CHA), while community benefit programs in the past tended to be planned and carried out by the hospital itself, today’s programs work with a wide range of community partners to improve community health and increase access to services. Additionally, community benefit programs are more public health oriented, using tools and expertise from professional and academic public health. To ensure community benefit programs are creating a sustainable impact, hospitals are strategically focusing resources on issues where they are likely to make an impact, rather than attempting to create change in a variety of areas with limited success. To make informed choices about the programs that will be most beneficial to the community, hospitals must conduct a community health needs assessment.
Community Health Needs Assessment and Community Health Improvement Plan
The CHNA is the means through which hospitals set out to identify the community’s needs. The CHNA is a discovery process by which an organization may identify and then prioritize the needs of the community that it serves.
The first step in this process is to identify and define the hospital’s community. This is determined by the geographic service area and populations served within that area. Some questions to ask and answer when defining community include:
- Does the hospital serve several towns in a county, several counties in a state, or the entire state?
- Does the hospital serve a specific population in a geographic service area? For example, only individuals with behavioral health needs.
- Does the population include medically underserved, low-income, or minority populations?
The CHNA is based on an analysis of primary and secondary data. Primary data includes the data from the hospital regarding the patients it serves. Secondary data includes public health data from the local and/or state public health department. Significantly, input from “persons who represent the broad interests of the community” served by the hospital facility, including those with “special knowledge of or expertise in public health” is required. This input can be obtained through surveys administered to community members, focus groups, and key stakeholder interviews. When thinking about who constitutes a community member and key stakeholder, it is necessary to think broadly. Members of the community includes not just the patients and their caregivers, but also includes local law enforcement, local health departments, employers, community-based social services organizations, and the Chamber of Commerce. The key stakeholders should have a basic knowledge of the work done by the hospital and an intimate knowledge and understanding of the community in order to answer in-depth questions.
All of this information, data, and input is assessed and analyzed so that significant health needs in the community can be identified. When identifying significant health needs, the hospital “may use any criteria to prioritize the significant health needs it identifies, including, but not limited to:
- the burden, scope, severity, or urgency of the health need;
- the estimated feasibility and effectiveness of possible interventions;
- the health disparities associated with the need; or
- the importance the community places on addressing the need.”
Not only is it important to identify the needs in the community, but also the resources available in the community and the capacity of those resources to meet the level of need in the community.
With the needs identified and supported by data, resources within the community and an understanding of gaps in resources, the hospital is now ready to determine how it will address these needs. These initiatives are documented in the Community Health Improvement Plan (CHIP).
The CHIP is a long-term strategy that spans three years and is meant to address the needs of the community as identified by the CHNA. The Plan should be used by the hospital in collaboration with community partners, to set priorities and coordinate and target resources. A CHIP is critical for developing policies and defining actions to target efforts that promote health. It should define the vision for the health of the community through a collaborative process and should address the gamut of strengths, weaknesses, challenges, and opportunities that exist in the community to improve the health status of that community.
Specifically, the CHIP includes goals with specific metrics that the hospital must be prepared to monitor and meet. It also includes supporting documentation spanning the three-year process which shows progress in achieving the established goals.
Monitoring and Reporting Community Benefit
As previously noted, hospitals must report community benefits on the IRS 990 form, Schedule H. Schedule H standardizes what counts as a community benefit and requires nonprofit hospitals to provide specific information about their policies and practices relating to community health needs assessment, financial assistance, hospital charges, billing and collections, and the other requirements for charitable hospitals.
This reporting requires more than just a simple accounting of dollars spent on these activities. The ACA added the requirements that hospitals must also “evaluate the impact” of their activities by demonstrating outcomes from initiatives as described in their prior implementation plan and to report on these activities every year on Form 990 Schedule H. Hospitals must therefore ensure that they are collecting and monitoring the necessary data to fulfill all the requirements of Schedule H.
The collection and monitoring of data should begin with the CHNA, continue during execution of the CHIP with regular assessment of metrics, and result in annual reports required by the IRS. While reporting to the IRS is a matter of compliance and an important focus of the work, the ultimate priority should be to ensure that the initiative or program is achieving the desired goals. Therefore, best practice indicates that such projects should incorporate continuous quality improvement to ensure the best outcomes over the course of the three-year CHIP. As CHIP strategies and activities may not have the intended impact, resource availability may change, and/or new research can yield useful insights.
Continuous quality improvement (CQI) requires ongoing monitoring of data and adjustments to initiatives. Underlying a strong CQI program is an infrastructure that allows for real-time access to data and the ability to manipulate and disaggregate that data for ongoing monitoring activities. Systems and software have been specifically designed to accommodate hospitals engaging in CHNA/CHIP activities and may utilize different platforms and include a variety of bells and whistles. We have identified the following as key components for such a data system:
Integrated data. The ability to have access to an integrated view of the data throughout the entire CHNA/CHIP process is key. An integrated view of the data ensures that the activities and metrics tracked in the CHIP can be tied back to the populations assessed in the community and the needs that the initiative is intending to address. While this process can be managed across multiple systems there is an increased risk of data errors.
Real-time access. Secondly it is advantageous to have real-time access to data. Data lags that only allow monitoring to occur quarterly or annually limit an organization’s ability to quickly adapt to findings through CQI.
Accessibility and Transparency. Accessibility and transparency are important functions of any data management system that would be utilized to track community benefits. Accessibility ensures that hospital staff who are participating in the initiative and gathering the data can easily utilize the system to enter data and retrieve data. Transparency is key to providing broad visibility to the data when engaging in collaborative efforts with partners outside of the hospital. Dashboards and charts to demonstrate progress over time are examples of tools that enhance the transparency of initiatives through shared data.
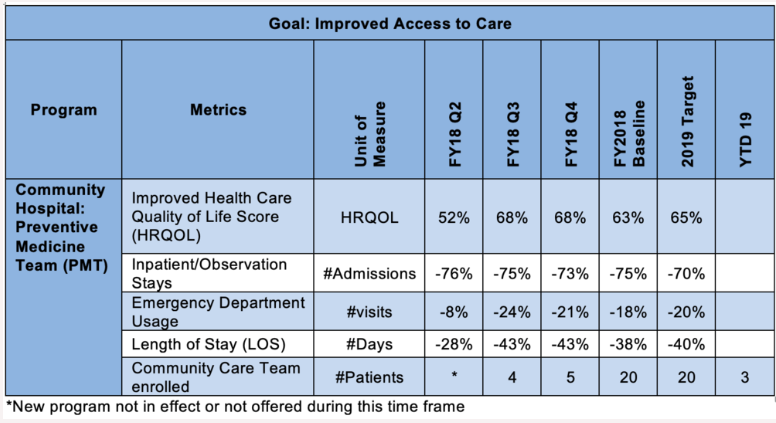
The dashboard below is an example of what a hospital may use to monitor progress towards a goal for a specific community benefit program. There are alternative tools available for hospitals that cannot afford to purchase access to a comprehensive software or system, such as the Community Benefit Reporting Tool created by the Rural Hospital Performance Improvement (RHPI) Project.
Potential Challenges and Pitfalls to Maximizing the CHNA and CHIP Processes
While nonprofit hospitals are required to document community reporting, it is also within the best interest of the hospital and the communities served that activities being conducted to improve the health of the community are achieving goals and resulting in improved outcomes. We have identified some common challenges and barriers that may inhibit hospitals’ ability to maximize the CHNA and CHIP processes and provide some insights as to how hospital leadership might address these issues.
In order to assure that staff are actively participating and documenting community benefit occurrences, it is necessary to be mindful of and have plans to meaningfully address potential barriers. The first is that many staff often feel over worked and overwhelmed. For them, the thought of doing supplementary activities is often more than they can handle. Secondly, there may be staff who go above and beyond and are very actively involved in Community Benefits, but who do not understand the significance of documenting these activities in the tracking system and do not take the time to do so.
How do hospitals identify and meaningfully engage staff that want to participate in and report on community benefit activities? A good first step is to make sure staff fully understand the importance of Community Benefits. It’s essential that the entire staff knows why a nonprofit hospital carries out these activities. One way this point can really be driven home is to help the staff understand the financial repercussions should the hospital fail to demonstrate its community benefit. Another is to show how providing community benefit furthers the mission of the hospital and the impact it has on the wellbeing of the community.
Ongoing training and incentives should be provided to achieve a long-term commitment to community benefit activities. To do this, the hospital’s Community Benefit Department must be prominent within the organization and its leadership. This department is the hospital’s best resource for all staff as they can answer questions and encourage staff commitment in a meaningful way. Additionally, all Community Benefit trainings, as well as the final review and approval of all occurrences, should be done through this department under the guidance of well-trained staff and knowledgeable leaders.
In our experience, quarterly trainings tend to be the most effective. Trainings can be developed and provided in-house or you can partner with Atrómitos to provide the trainings. With the support of our policy and operational experts and communications specialists, Atrómitos has the expertise and resources to create customized training materials to support your CHNA/CHIP programs. This support may include live and/or recorded web-based trainings to provide initial as well as ongoing training to staff at all levels of the organization and partners/collaborators as needed. In addition, Atrómitos develops training guides and desktop references that can be posted to internal human resources systems providing easy access to step-by-step directions on important skills and concepts such as entering data into your tracking system. Finally, to ensure the effectiveness of trainings, Atrómitos develops short assessments that can be administered during or after training activities to determine whether the concepts were understood and mastered.
Another way to assure staff report their Community Benefit activities is through incentives. Atrómitos can assist in the development of such incentives which may include hospital-wide recognition of individuals who have demonstrated significant commitment to the community through their community benefit activities. This recognition can be made monthly in internal newsletters, quarterly at leadership meetings, and/or annually through a Community Benefit award. By recognizing staff commitment to Community Benefits, hospital leadership reinforces the importance of supporting the community. In addition to recognition programs, can work with your human resources department to design more tangible incentives which can include extra paid time off, a donation to the staff member’s charity of choice, or gift certificates. Such incentive programs would be designed to not only encourage participation in community benefit activities, but also the reporting of activities and data in the hospital’s tracking software.
Finally, leading through example is often the most effective means to encourage staff to participate in and report community benefit activities. It is crucial that leadership gives back and actively participates in Community Benefit activities – and reports the activities!
With a thorough understanding and commitment to community benefits from all staff and leaders, hospitals are not only able to fulfill the IRS requirement, but most importantly, are able to make significant strides in improving the health and wellbeing of the communities they serve. At Atrómitos we have the resources to assist in all aspects of community benefits including Community Health Needs Assessment, Community Health Improvement Plan, Community Benefit reporting trainings and workshops, and Community Benefit incentive programs.


