Earlier this month, the North Carolina Department of Health and Human Services (NC DHHS) issued its latest Medicaid Managed Care Policy Paper describing a new element of Medicaid Transformation in the state. In this paper, NC DHHS announced its intent to establish a specialized managed care plan for children in foster care, adoption support, and individuals under the age of 26 who were formerly in foster care (for ease I’ll refer to this group collectively as children in foster care).
In my discussions with key stakeholders about this plan, I have learned that some were surprised by this development. While Medicaid Transformation has been in process for some time (and I can see how some details have been forgotten), NC DHHS included the creation of such a plan in its 1115 waiver application to the Centers for Medicare and Medicaid Services (CMS).
Some Background
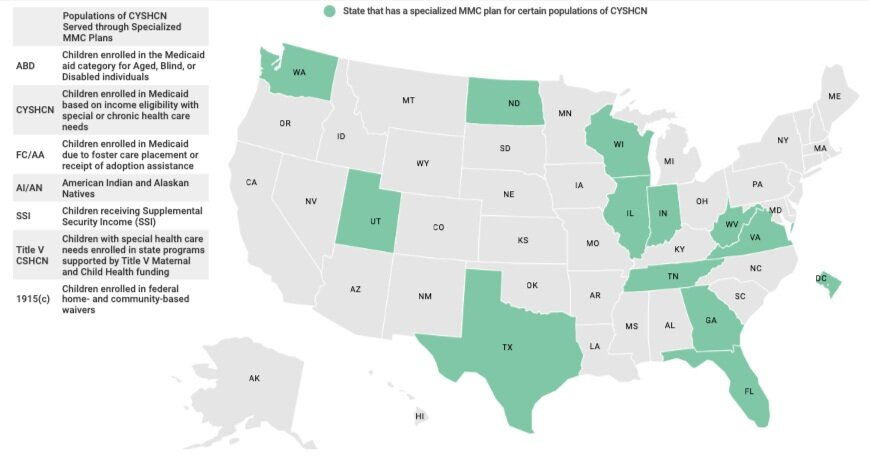
The use of specialized managed care plans for children and youth with special health care needs (CYSHCN) who are enrolled in Medicaid is not a new concept. Other states have used such plans to meet the specialized needs of these children for quite some time. However, there has been a rapid escalation of the number of states using such plans. As an example, when the National Academy for State Health Policy (NASHP) conducted its study of states using specialized plans for children in foster care in 2017, only two states were doing so. Just two years later in 2019, nine states had such plans.
Texas has the most experience providing specialized coverage through a single, statewide managed care plan for children in foster care, having established its program, STAR Health, in 2008. Texas’ program has many similarities to the program proposed by NC DHHS. With its long operations, there are many lessons that can be learned by NC DHHS for use in its own implementation.
I’ve had the unique experience of leading a team charged with developing a foster care program for a state affiliate of a national Medicaid plan. Therefore, I can personally attest to the critical importance of developing a program that genuinely accounts for and addresses the widely varying and extraordinarily complex needs of children in foster care. These complex needs can vary from simply providing children with suitcases so that they need not pack their belongings in a trash bag when transitioning placements, to preventing the overutilization of anti-psychotic medications in such children.
Children in foster care often have many adults involved in the management of their wellbeing. However, each adult is often responsible for one or just a few aspects of the child’s wellbeing. There are case managers, legal guardians, biological parents, teachers, health care providers, and many others that each play important roles in the children’s lives. In the best of circumstances, the coordination and collaboration among all of these adults are limited, if it happens at all.
In its design of the Foster Care Plan (FC Plan), NC DHHS has (rightly) focused much attention on a care management model that the FC Plan will be required to deploy. North Carolina already has a few different programs in place to help improve coordination and collaboration among those responsible for meeting the needs of children in foster care, from the System of Care Framework to Fostering Health North Carolina, a medical home model for these children.
While NC DHHS states in the policy paper that the FC Plan “will also be required to align its care management approach with the North Carolina System of Care Framework…” it is unclear from the paper if and how the work of Fostering Health North Carolina will be continued and how that experience and infrastructure can be best leveraged in the new model.
In the rest of this particular article, I won’t go into detail on the care management model, but I will do so in our next article on this issue. This is because the care management model for the FC Plan is central to the success of the program and I want to give it the attention it deserves.
Instead, let’s begin with a focus on some other important points for stakeholders to keep in mind.
Eligibility for the FC Plan
NC DHHS defined the following groups as being eligible for the FC Plan:
- Children in foster care
- Children receiving Title IV-E adoption assistance
- Children formerly in foster care up to age 26 if they reside in NC, up to age 21 if they reside in another state
- Children of individuals who are eligible for the FC Plan
Until the FC Plan launches (expected July 1, 2022), those eligible for the FC Plan will remain in Medicaid Direct (fee-for-service) and, if applicable, the LME/MCO. NC DHHS intends to automatically enroll those eligible for the FC Plan into the plan effective July 1, 2022.
This is a process that will require particular care and attention, so as not to disrupt treatment that is underway or create complexity for guardians of children in foster care, who may need to take action to transfer enrollment to a different plan based on the child’s needs. This is because those eligible for the FC Plan may instead enroll in a Standard Plan, a Tailored Plan (if they meet eligibility), the Tribal Option, or they may opt to return to Medicaid Direct.
What NC DHHS Must Do
First, the General Assembly needs to enact legislation that allows for the creation of the FC Plan and for the enrollment of eligible individuals into the plan. NC DHHS is currently working with the General Assembly to obtain the needed legislation. Then, NC DHHS will need to procure the FC Plan.
NC DHHS intends to issue the FC Plan procurement this Spring, with the selection of the successful bidder this coming Fall and a go-live date of July 1, 2022, as previously mentioned. Only organizations that are currently a Standard Plan or a Tailored Plan are permitted to apply to be the FC Plan. While the Tailored Plans are currently being procured, we know that only the existing LME/MCOs are permitted to apply for the Tailored Plan program. Therefore, we can expect that the Tailored Plans will be some, if not all, of the existing LME/MCOs, including:
- Vaya Health
- Trillium Health Resources
- Sandhills Center
- Partners Behavioral Health Management
- Eastpointe
- Cardinal Innovations Healthcare Solutions
- Alliance Behavioral Healthcare
Furthermore, we do know who the Standard Plans are:
- Healthy Blue (Blue Cross Blue Shield NC) (statewide)
- Carolina Complete Health (Medicaid Regions 3, 4, and 5)
- UnitedHealthcare Community Plan (statewide)
- AmeriHealth Caritas of North Carolina (statewide)
- WellCare of North Carolina (statewide)
While all of the contracted Standard Plans (and, likely, Tailored Plans) have at least some experience covering children in foster care, some plans certainly have more experience than others. Centene (the plan behind Carolina Complete Health ) is one such plan with more experience, as it is the only plan that has been contracted in Texas for STAR Health since 2008.
What the Plans Must Do
Next, the provider network of the FC Plan will need to have not only primary care doctors but also adequate specialists, all of which will need to be trained on Adverse Childhood Experiences and Trauma-Informed Care.
The FC Plan is required to have an open network and to contract with any willing provider. Network adequacy requirements will apply and, while the requirements will be similar to those required of Standard Plans and Tailored Plans, there will be some differences as well. NC DHHS has not yet specified those standards.
Rate floors will apply, as they do with Standard Plans, in that the FC Plan cannot pay in-network providers below 100% of the Medicaid fee schedule. Providers that are out of network cannot be paid more than 90% of the Medicaid fee schedule, except for emergency services, post-stabilization services, and services during transitions of care, which must be paid at 100% of the Medicaid fee schedule.
Lastly, NC DHHS has identified the need for the FC Plan to have staff that understands and has experience with the unique needs of children in foster care. Key leadership positions that are required include:
- A Chief Medical Officer who must be either a licensed pediatrician or family physician with a minimum of seven years working with children in a clinical setting.
- A Deputy Chief Medical Officer who must be a licensed child and adolescent psychiatrist with a minimum of five years of clinical experience and two years’ experience in managed care.
- A Director of Population Health and Care Management who must be a fully licensed clinician with a minimum of five years of demonstrated care management/population health experience in a health care organization serving Medicaid beneficiaries.
- A Pharmacy Director, who is a North Carolina, registered pharmacist with demonstrated experience in medication management for high-risk children, including children in the child welfare system, and at least three years experience with Medicaid pharmacy benefits management.
All staff must reside in North Carolina and have trauma-informed care experience.
What Partners Must Do
For providers contracting with Standard Plans or Tailored Plans, I recommend you understand if the plan intends to participate in this product. If so, you should also understand how your contract with the PHP will or will not be used by the plan to include you in an FC Plan network.
This is important for a variety of reasons, not the least of which are the quality measures that the NC DHHS will use in the FC Plan. While NC DHHS intends to align the measure set across the types of plans, the special needs of children in foster care will necessitate some differences in measures.
This could be achieved in the addition of these measures to the existing priority measure set or by replacing some existing measures with different measures. Understanding this is important not just from the perspective of understanding what providers will be required to report as well as the performance targets that will be expected, but also for value-based payment arrangements. Providers should understand if the plans will issue a separate VBC addendum for the FC plan or if the population will be included in an existing VBC addendum.
Other components important to providers include:
- Care management will be provided by the plan. This means that providers that are AMH Tier 3 providers or LHDs providing care management to at-risk children will need to understand how these programs will interact, collaborate, and coordinate.
- Providers that are Advanced Medical Homes may be eligible for additional payments if the practice meets other (yet to be specified) requirements beyond those that apply to the AMH program (current Carolina ACCESS requirements).
- Providers involved in the care of children enrolled in the FC plan will be eligible for a fee-for-service payment for participating in care team meetings with the FC Plan care managers. This is a significant (and very smart) design feature of the FC Plan, one of the biggest challenges for care managers is and always has been getting providers to participate in care management team meetings.
Implementation of a Foster Care Plan may be just what is needed to create a system-wide collaboration that meets the complex needs of children in foster care. However, doing so will require meaningful stakeholder involvement.
I encourage all stakeholders to get involved and provide meaningful input to NC DHHS and for NC DHHS to be receptive to this feedback. Children in foster care already have complicated lives. We, as a society, have already let them down in many ways. Let’s take advantage of this opportunity to collectively effect change and improve the lives of these children.


