The extreme weather of January 2022 has left many of us dreaming of sunnier, dryer days. It is therefore with great anticipation that I await February 2nd and the predictions of Punxsutawney Phil.
“This is one time where television really fails to capture the true excitement of a large squirrel predicting the weather.”
Thanks to the king of droll, Bill Murray, I can’t hear mention of Groundhog Day and not think about the epic predicament that Phil Conners faced in the movie. I am certain that like Phil we would all react negatively if forced to repeat a single day of our lives over and over and over again. Let’s be honest the pandemic has certainly made this scenario feel a bit more real for all of us recently. And while simply watching this movie can improve one’s mood there are many deeper lessons that can be learned from Phil’s existential experience. The one that speaks most loudly to me during this time of great isolation and solitude is the importance of trying to connect with people and make friends. As it was those connections with others that ultimately changed the course of Phil’s day and lead to his escape of Groundhog Day.
At this point you are likely thinking, “I love Bill Murray and all but how in the world does this connect to National Patient Recognition Week”? To me it’s quite simple, across the healthcare sector we are all seeking to make change, real change, big change that leads to improved outcomes and reduced costs. Many of us are developing new provider partnerships, digging deeper into data, and agreeing to new payment mechanisms. This is all important, but these strategies will not be enough if we don’t recognize the patient and their roles in reforming our system from one that provides reactive health delivery to creating more efficient, effective, and equitable environments of health. Healthcare is predicated on patients and the patients must be a part of any change.
Like Phil, if we don’t look beyond ourselves (providers and payers) we will not be able to achieve the change we are so desperately seeking.
Now I am not suggesting doctors and other healthcare providers become friends with their patients, but I am going to suggest that we make significant changes to the provider-patient relationship. Healthcare is a consumer-based market, yet it is the sole sector where the buyer (patient) is in an asymmetrical power relationship with the seller (doctor). The doctor-patient relationship is built on a paternalistic model with a long history. Where the patient seeks help from the all-knowing doctor whose decisions are silently complied with. While the dynamic has been shifting with the advent of the patient-centered care movement, we have a long way to go!
In honor of National Patient Recognition week, I propose that we seek to improve our relationships with patients by establishing a foundation of trust. While many surveys and metrics (and in some cases dollars) in healthcare today focus on patient experience and patient satisfaction, trust is paramount to the strength of any relationship. “Without trust” as the saying goes “you have nothing.” Earning, maintaining, and reinforcing trust should therefore be the foundation of any and every patient interaction. And we should remember this principle any time we seek to improve those metrics related to patient experience and satisfaction, but also to patient adherence and clinical outcomes
Before we can build trust, we need to understand where we stand with patients today. The American Board of Internal Medicine Foundation commissioned NORC at the University of Chicago to conduct the Surveys of Trust in the U.S. Health Care System. The 2020 report found that only 64% of respondents trust the healthcare system in general. And while overall trust of clinicians specifically is greater (85%) disparities persist. Black (71%) and Hispanic (68%) consumers report lower levels of trust in their primary care physicians than White consumers (82%). And because trust is a two-way street, it is important to note that only 83% of respondents believed their doctor trusted what they said. Whereas 98% of surveyed physicians believed that their patients trusted them. Suffice to say that is a pretty significant disconnect.
If these numbers alone do not convince you that it is time to work on our collective trust issues, we also know from 2017 peer-reviewed research that patients who have more trust in their healthcare professionals are more satisfied with their treatment, have fewer symptoms, and pursue healthier behaviors. Other studies have shown that trust is a strong predictor of a patient continuing with their provider. All signs point to trust in the patient-doctor relationship is of benefit to all parties.
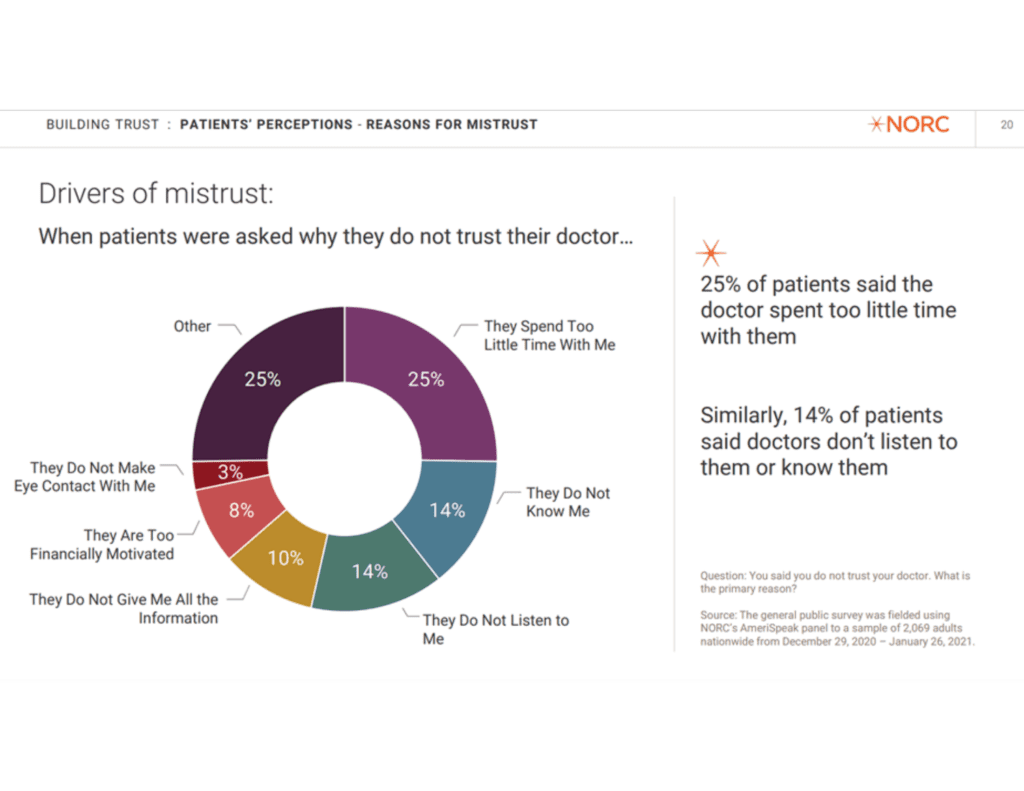
So how do we as leaders in healthcare move down the path of behavior change from contemplation to preparation and ultimately start building trust with patients? Leveraging the data from the NORC study we can better understand the perspective of the patient and begin to address their concerns.
Build Rapport with your Patient
I understand that building a rapport takes time and it may seem to fly in the face of the number one complaint of patients in the survey (they spend too little time with me) that I am suggesting you take time from your limited visit to build a rapport with your patients. But if the answer is that you don’t have more time (which I expect it will be) consider that if you spend a small amount of time making your patient feel like they are seen and heard (#2 and #3 on the list) it is very possible that they will feel like the time though limited was sufficient and constructive. It can be a question of quality in the absence of that limited resource of quantity. Thus, building trust in the relationship.
The American Academy of Family Physicians has developed Tips on Building Doctor/Patient Relations and includes a number of strong recommendations for building rapport with your patient.
Screen for and address your Patient’s Social Determinants of Health
Given the clear evidence that the social determinants of health (SDOH) account for between 30-55% of health outcomes, it behooves organizations to implement screening processes that assess patient need in these areas. While these screenings most often occur outside of the doctor-patient interaction, it is important that clinicians are taking the time to discuss SDOH needs with their patients. Not only will this move the needle on health outcomes for your patient, but it will also demonstrate to them that you know them (beyond their medical diagnosis) and thus build trust in your relationship with your patient.
Informed by two years of research, Stanford researchers developed five evidence-based recommendations that clinicians can take to be fully engaged with patients and understand their perspectives, life circumstances, and priorities.
The importance of SDOH shouldn’t be underestimated when it comes to engaging with a patient and managing their conditions. This is not only because of the direct, demonstrated association between SDOH and outcomes, but also because it is an application of meeting your patient where they are at and seeing them for the totality of their experience and environment. SDOH must matter to providers because they matter to their patients.
Engage your Patient on the Team
The Cleveland Clinic proactively and systematically categorized all patient comments from their patient satisfaction surveys over a nine-month time frame pre-COVID-19 pandemic. One of the common complaints highlighted that patients don’t feel part of their care decisions. This is something that must be corrected in order to provide quality, patient-centered care. Patient-centered care provides a model of care that puts the patient at the functional center of the team. The model ensures that regular engagement of the patient by the care team leads to improved outcomes and patient satisfaction.
While the pandemic initially exacerbated access challenges in healthcare, ultimately the relaxing of regulatory standards and a policy push for the expansion of telehealth, doctors, and patients have found telehealth and other technologies in some cases enhanced their ability to engage and communicate not only with patients but also with other members of the care team.
Educate your Patient to Improve Health Literacy and Self-Care
There is strong evidence to suggest that counseling and patient education provide substantial benefits. Providing patients with complete and current information helps create an atmosphere of trust, enhances the doctor-patient relationship, and empowers patients to participate in their own health care.
Education starts with a dialogue where the clinician elicits the patient’s thoughts, feelings, and beliefs, and then provides new information consistent with the patient’s needs and interests. This give and take ensures that the education/information shared acknowledges the unique needs of the individual and is personalized to meet the patient where they are at in terms of health literacy and ability to engage in self-care.
Increase Transparency
Studies tell us there is significant frustration about healthcare driven by a lack of awareness and understanding of the current system and its challenges. The general public does not understand the complexities inherent in the existing system and the magnitude of the forces that are seeking to change healthcare from a variety of angles, including regulations, payment mechanisms, technologies, and workforce. It is no wonder that a complex opaque system such as healthcare lacks the trust of the public.
The complexity and opacity of a health system and the navigation of clinical care is a point of concern in any system, but it is doubly important in the US health care system which is predicated (primarily) on free-market principles, relying upon the patient to operate as a savvy consumer of health services. This is a role that is difficult for any patient to play, all the more so when there is a lack of transparency, predictability, (seeming) rationale associated with the prices of health services.
While efforts are underway to bring transparency to hospital pricing, there is much work to do. And when it comes to building trust with patients, pricing transparency is just one piece of the puzzle. To truly gain patient trust there must be greater transparency in all aspects of the healthcare transaction. This means making standardized, comprehensible quality data accessible and that includes patient rankings of hospitals, doctors, and other providers.
In conclusion, and to return full circle, there are practical steps we can (and must) take to not only engage with our patients and cultivate trust, but place them, individually and collectively at the center of all health care and health system decisions. Because we are looking for big change here, a new day – a different day, we are looking to get to the happy ending of this groundhog day when in the words of Phil Connor’s we can say: “Today is tomorrow. It happened.” That only happens together.
